 The Centers for Medicare and Medicaid Services (CMS) just released the final 2013 open enrollment data for Medicare Part D Prescription Drug Plans (PDPs). These updated data include about 1 million additional seniors and show some slight differences versus the initial data release.
The Centers for Medicare and Medicaid Services (CMS) just released the final 2013 open enrollment data for Medicare Part D Prescription Drug Plans (PDPs). These updated data include about 1 million additional seniors and show some slight differences versus the initial data release. However, the song remains the same. As I note last month, 16 of 2013's 190 PDPs have a preferred pharmacy network design. Consistent with the preliminary numbers, more than 4 out of 10 seniors enrolled in one of these 16 plans. Walgreens will benefit from active participation in preferred networks. CVS Caremark’s retail business will face headwinds. See the updated data table and comments below.
While consumers have been showing a whole lotta love for preferred networks, you may think that CMS has been standing around like a fool in the rain. But last week’s 2014 CMS call letter unexpectedly announced that CMS is now “concerned” about potentially higher costs in preferred networks. Check out the surprising excerpt below.
OVER THE HILLS AND FAR AWAY
To get data on PDP enrollment, ramble on to this CMS page: Medicare Advantage/Part D Contract and Enrollment Data. http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/MCRAdvPartDEnrolData/index.html
In Brand New 2013 Part D Data: Nearly Half of Enrollees Chose Preferred Pharmacy Networks, I analyzed the first data release, which covered enrollments accepted through December 5, 2012. This original article has links to each plan’s home page.
The open enrollment period ended two days later, on December 7, 2012. The new data cover enrollments through January 11, 2013, and include an additional 967,111 people (+4.5%). Of these new enrollees, 190,863 (19.7%) signed up for a PDP with a preferred pharmacy network.
WHEN THE LEVEE BREAKS
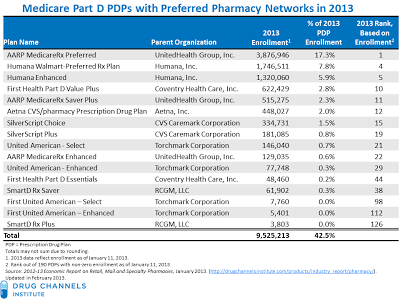
There were 190 PDPs with non-zero enrollment as of January 11, 2013. Total PDP enrollment was 21.5 million people. The 16 plans with preferred pharmacy networks enrolled 9.5 million people, or 42.5% of the total. Here’s an updated summary of the 16 PDPs with preferred pharmacy networks:
Observations and updated scorecard:
- Humana-Walmart wins again. The Humana Walmart Preferred Rx Plan, which launched in October 2010, is the second-largest PDP with a preferred pharmacy network and the fourth-largest PDP, with 7.8% of total PDP enrollment. There’s been no communication breakdown with consumers—total enrollment has increased by 355,279 seniors (+25.5%) since January 2012.
- Walgreen joined the preferred bandwagon. In 2013, Walgreen gave no quarter by wisely deciding to be a preferred pharmacy in the Coventry, Humana, UnitedHealthcare, and SmartD plans. In 2013, plans with Walgreens as a preferred pharmacy account for 29.3% of total PDP enrollment, and 69.1% of preferred pharmacy network PDP enrollment.
- CVS stayed out of the preferred networks. CVS retail pharmacies are in only the Aetna/CVS and Silverscript plans. In 2013, plans with CVS as a preferred pharmacy account for 4.3% of total PDP enrollment, and 10.1% of preferred pharmacy network PDP enrollment. This result was nobody’s fault but theirs. The Aetna CVS/pharmacy Prescription Drug Plan boosted year-over-year enrollment by 116,808 (+35.3%).
- Walgreen’s SmartD plan was a heartbreaker. The SmartD Rx plans attracted a mere 65,705 seniors, or 0.3% of total PDP enrollment. These plans are offered by RxAlly, a new pharmacy group that claims to have about 14,000 independent pharmacies plus Walgreens drugstores. Walgreen is the major investor behind RxAlly and SmartD. On the plus side, the plan added 20,000 seniors from December 5 to January 11.
WHAT IS AND WHAT SHOULD NEVER BE
CMS’ 2014 Call Letter, released on February 15, provides information that Medicare Advantage Organizations (MAOs) and Part D sponsors need to take into consideration in preparing their 2014 bids.
On page 157 of the 2014 Call Letter, CMS writes:
“We have begun to scrutinize Part D drug costs in PDPs with preferred networks, and comparing these to costs in the non-preferred networks, as well as to costs in PDPs without preferred networks. We are concerned because our initial results suggest that aggregate unit costs weighted by utilization (for the top 25 brand and top 25 generic drugs) may be higher in preferred networks than in non-preferred networks in some plans. Combined with lower cost sharing, we believe these higher unit costs may violate the requirement not to increase payments to such plans.” (emphasis added)Hmmm, this is an unexpected twist. CMS states that it “…will be contacting the plan sponsors identified in our analysis to validate our findings in the near future.” PDPs better watch out, or they’ll be trampled under foot.
P.S. Guess who just bought Celebration Day?

"This result was nobody’s fault but theirs".
ReplyDeleteAdam, I wouldn't be so certain about this re CVS and preferred PDP networks.
I own a small indy drugstore and I requested well in advance to become preferred with certain PDP's. Not surprising, I rec'd the standard reply of "I'm sorry but we're complete at this time"....and this was 9 months before the new Med-D year started!
I'd say that the narrow network phenom gave CVS a pinch of their own medicine.
And I realize the wheels of gov often move slow, but it finally looks like any willing provider will replace "preferred" providers this upcoming year. (At least that's what I'm hearing).
After reading that I’m dazed and confused
ReplyDeleteFYI, the sentence you quoted was one of the Led Zeppelin easter eggs in today's post.
ReplyDelete;)
Don't know where you're goin', only know just where you've been?
ReplyDeleteYeah, I know the feeling.
does the government really think these plans or pbms do anything other than to benefit themselves,, For sakes this is a FOR PROFIT industry ( insurance)
ReplyDeleteOfcourse they will charge higher to the plans. Its makes perfect sense. There is only so much lower you can get a brand name drug.
Nicely deployed theme…ejoyed it. But whenever they get to the bonham of this I’ll plant my focus back on your page jones’n for better understanding of it
ReplyDeleteFYI the lawsuit against cvs caremark filed in texas moves ahead in court. Its going to be an interesting one for CVS.
ReplyDeleteouch.
ReplyDeleteOK, I did appreciate the wall to wall references to Led Zepplin, esp. with more talk (yet again) of a re-union, the first since the Dec 2007 concert on the wrong side of the Pond.
ReplyDeleteMy kids say I'm a music fool. I must have been taking it the wrong way all these years!
ReplyDeletehttp://www.latimes.com/business/money/la-fi-mo-anthem-drugs-20130219,0,581809.story
ReplyDeleteGuess a bit push back on these preferred network which only has ONE pharmacy in it!!
Another great blog on Pref networks in D. Did you notice page 148 of the adv notice? I'm wondering who cms was aiming that comment at.
ReplyDeleteYes, I noticed that comment. In Medicare Part D, pharmacies typically pay a $1 to $3 per-prescription fee to the plan to participate in a preferred network. on page 148, CMS is questioning the accounting for those fees and impact on beneficiaries. CMS stated: "Upon consideration, we believe that any such post-point-of-sale claim adjustments violate our current guidance on negotiated prices."
ReplyDeleteI suspect CMS will issue sub-regulatory guidance that may change how Part D sponsors and pharmacies interact in plans with preferred pharmacy networks.
Everyone here except pharmacy owners seem to know what games these pbms play. Its one to read about it but another to see it for yourself. Its quite remarkable to see it actually. I shall give you an example..just today a patient who gets maintaince meds from the largest PBM's mailorder wharehouse came in with a bill from two weeks ago that showed how much was billed to his insurance. I was floored to say the least. This patient has limited benefits so by the end of the year he is paying the full contract rate once all benefits are used up. First was generic lipitor. The pbm charged his plan 143 dollars for a 3 months supply and him a 5 dollar copay. So i ran the same drug under his wife's name for a 30 days supply. The copay came back at 12.93 cents, and guess what thats the total cost of the rx was. Nothing else being paid by the pbm. Another was generic diovan hct.. his mailorder billed him 345 for a 3 months plus 5 dollar copay. My reimbursement...84 dollars with a 15 dollar copay for a 1 month . Omeprazole 72 dollars was the cost for a 3 months from pbm mailorder.. mine 16 dollars .
ReplyDeleteRemember this family is on limited benefits, so one way or the other there paying for it. Sure there copay is less but pbm is eating away at the mans limited benefits. Adam if you would like to see these transactions..just let me know.
regards