- Hospitals earn incredible markups on CAR-T therapies
- Utilization management booms
- Health plans often ignore clinical guidelines
- Benefit designs flummox physicians
P.S. Please join the more than 13,100 consumers of my daily commentary and links to neat stuff at @DrugChannels on Twitter. You can also find my daily posts on LinkedIn, where I have more than 22,000 followers.
CARTwheeling the profits; large hospitals mark-up CAR-T therapy by $0.5M, Ronny Gal, Sanford C. Bernstein & Co.
Chimeric antigen receptor (CAR) T-cell therapy has produced amazing therapeutic breakthroughs. But who is profiting from these novel treatments?
Ronny Gal and his team at Sanford C. Bernstein have the answer. They examined the reimbursements that commercial health plans paid to hospitals for three CAR-T products: Kymriah, Yescarta, and Tecartus. The team relied on third-party payment data from 10 hospitals, which disclosed this information due to CMS’s Hospital Price Transparency rule. (I highlighted Ronny’s analysis of the oncology market in my September news roundup.)
The chart below tracks each CAR-T therapy by:
Three conclusions jump out:
Ronny Gal and his team at Sanford C. Bernstein have the answer. They examined the reimbursements that commercial health plans paid to hospitals for three CAR-T products: Kymriah, Yescarta, and Tecartus. The team relied on third-party payment data from 10 hospitals, which disclosed this information due to CMS’s Hospital Price Transparency rule. (I highlighted Ronny’s analysis of the oncology market in my September news roundup.)
The chart below tracks each CAR-T therapy by:
- the Wholesale Acquisition Cost (WAC) list price, which is set by the manufacturer
- the hospital’s chargemaster list price, which is set by the hospital
- the negotiated average payment, which is established in agreements between a hospital and a commercial health plan
[Click to Enlarge]
Three conclusions jump out:
- Hospitals mark up the list price by 300% or more. For instance, the average chargemaster price for Yescarta is $1,275,000—equal to 320% of the manufacturer’s list price of $399,000.
- Commercial plans pay hospitals more than twice the list price. The negotiated rates are -23% to -32% below the chargemaster price. Hospitals earn additional payments for medical services associated with CAR-T therapy treatment and administration.
- Hospitals absorb two-thirds or more of the funds that health plans pay for CAR-T. Hospitals purchase products below the WAC, due largely to 340B Drug Pricing Program discounts. For CAR-T, the hospitals’ mark ups and share of payments is consistent with that of other buy-and-bill products—but the dollars are much, much larger.
Utilization Management Trends in the Commercial Market, 2014–2020, Avalere Health
It's not your imagination: Insured patients are having more trouble accessing prescription drugs.
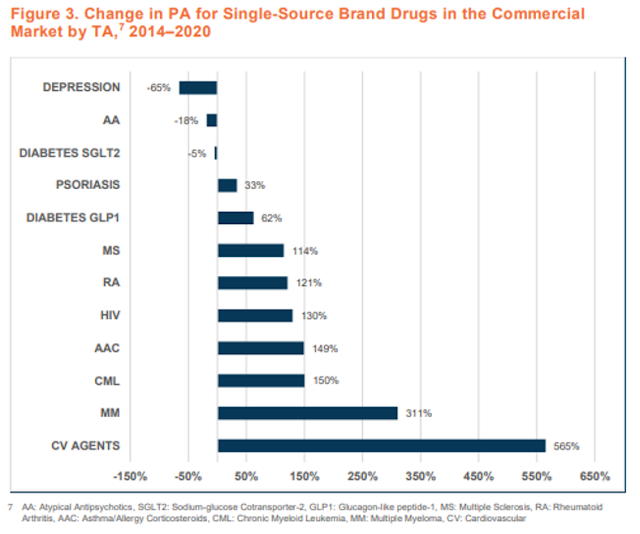
This Avalere Health study examined PBMs’ utilization management (UM) techniques—prior authorization and step therapy—for single-source, brand-name drugs.
For 2020, UM was most prevalent for specialty drugs that treat oncology and autoimmune disorders, and it was least prevalent for drugs treating mental health and other chronic conditions. What’s more, the use of UM has increased significantly from 2014 to 2020, per the report’s Figure 3 (reproduced below).
This Avalere Health study examined PBMs’ utilization management (UM) techniques—prior authorization and step therapy—for single-source, brand-name drugs.
For 2020, UM was most prevalent for specialty drugs that treat oncology and autoimmune disorders, and it was least prevalent for drugs treating mental health and other chronic conditions. What’s more, the use of UM has increased significantly from 2014 to 2020, per the report’s Figure 3 (reproduced below).
[Click to Enlarge]
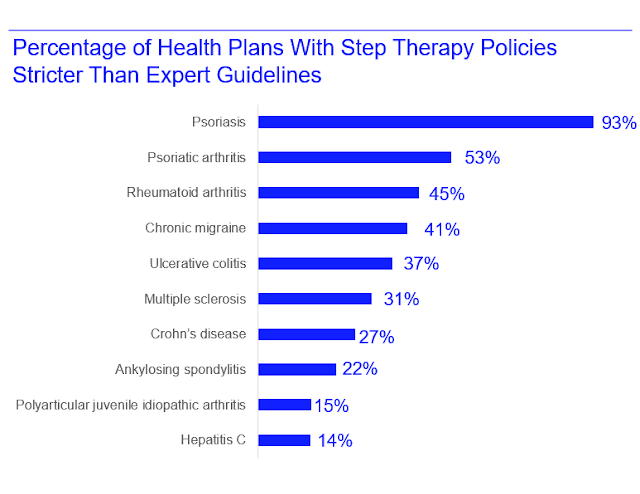
Variation In Use And Content Of Prescription Drug Step Therapy Protocols, Within And Across Health Plans, Health Affairs
Here’s an illuminating corollary to the study above: Health plans' step therapy rules are often more stringent than clinical recommendations. The step therapy rules also varied significantly across plans. Is this how health insurance should work?
The data below appear in the study’s Appendix Exhibit E. Thanks to Gary Karr at Real Chemistry for the chart.
The data below appear in the study’s Appendix Exhibit E. Thanks to Gary Karr at Real Chemistry for the chart.
[Click to Enlarge]
Accuracy of Physician Estimates of Out-of-Pocket Costs for Medication Filling, JAMA Network Open
In Employer Pharmacy Benefits 2021: Patient Specialty Costs Rise with Coinsurance and Accumulators, I reviewed the complex structure of pharmacy benefit designs. They’re why many of us struggle to compute our out-of-pocket prescription costs.
One tip: Don't ask your physician. They are also confused.
Per this JAMA study: “In this survey study of 371 primary care physicians, gastroenterologists, and rheumatologists, only 21% could accurately estimate out-of-pocket drug costs using information about the drug’s price and an insurance plan’s cost-sharing mechanisms, including deductibles, copays, coinsurance, and out-of-pocket maximums.”
The chart below highlights how few questions the physicians answered correctly. If well-educated MDs have trouble, how do you think patients feel?
One tip: Don't ask your physician. They are also confused.
Per this JAMA study: “In this survey study of 371 primary care physicians, gastroenterologists, and rheumatologists, only 21% could accurately estimate out-of-pocket drug costs using information about the drug’s price and an insurance plan’s cost-sharing mechanisms, including deductibles, copays, coinsurance, and out-of-pocket maximums.”
The chart below highlights how few questions the physicians answered correctly. If well-educated MDs have trouble, how do you think patients feel?
[Click to Enlarge]
How U.S. Health Insurance Works, Dr. Glaucomflecken
This hilarious video is depressingly accurate.



No comments:
Post a Comment